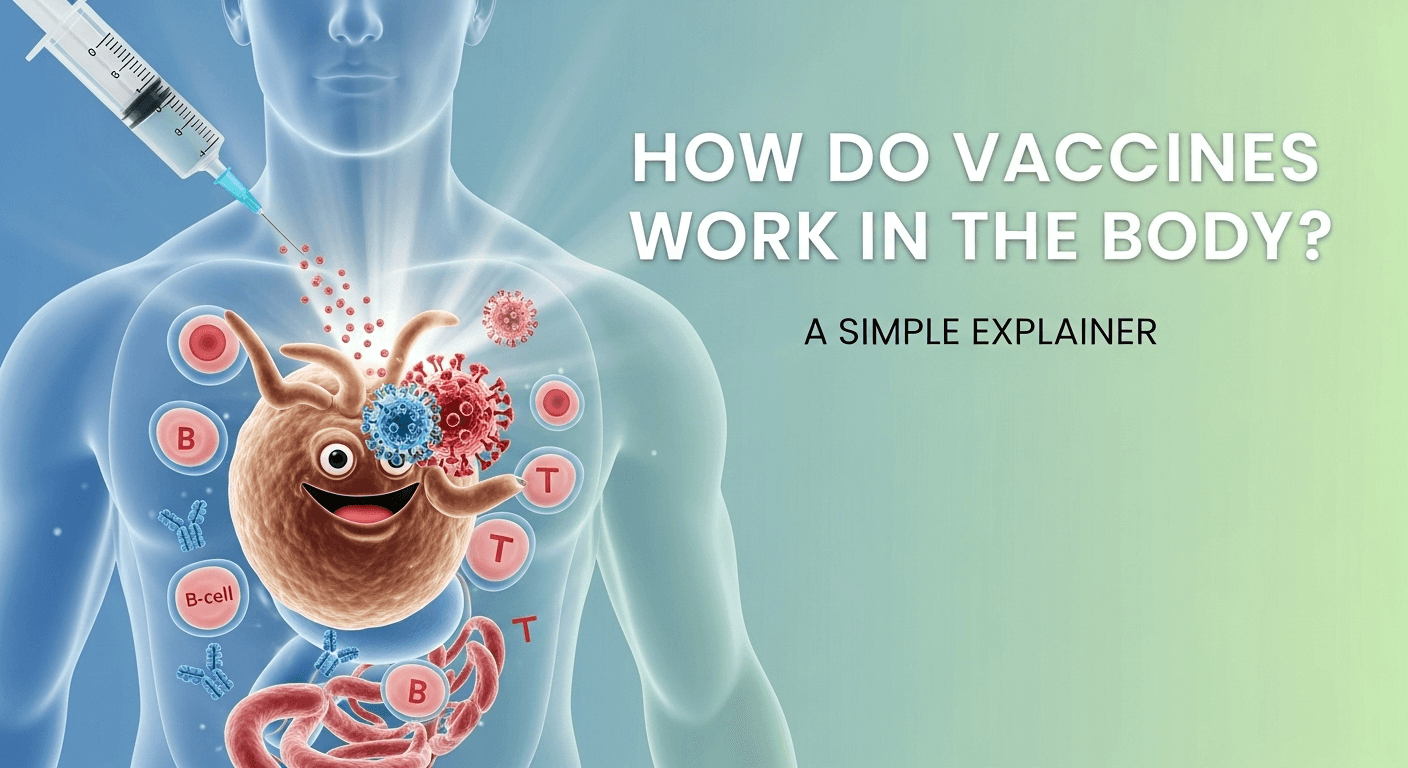
Vaccines are one of the greatest triumphs of modern medicine, a cornerstone of public health that has saved countless millions of lives from devastating diseases. Yet, for many, the process happening inside our bodies after an injection remains a bit of a mystery. You might have found yourself wondering, just how do vaccines work in the body to provide such powerful protection? The answer lies in a brilliant strategy: teaching our immune system how to fight a specific enemy before we ever encounter it in the real world. This article serves as a simple explainer, demystifying the elegant and effective science behind vaccination.
At its core, a vaccine is a biological training tool. It safely introduces your immune system to a harmless piece of a pathogen (like a virus or bacterium), or a weakened/inactivated version of it. This controlled exposure allows your body to build a “memory” of the invader without having to get sick first. Think of it as giving your body’s defense forces a detailed instruction manual and conducting a full-scale dress rehearsal. When the real pathogen eventually tries to invade, your immune system is not caught by surprise. It’s already primed, armed, and ready to launch an immediate, highly effective counter-attack, neutralizing the threat before it can cause serious illness.
This proactive approach is what makes vaccination so profoundly different from treatment. Instead of waiting for a disease to take hold and then trying to fight it off, vaccines empower our bodies to prevent the disease from ever establishing a foothold. It’s a testament to our understanding of the immune system’s remarkable ability to learn and remember. Over the next sections, we will break down this incredible process step-by-step, from the fundamental workings of your immune system to the different types of modern vaccines and the community-wide benefits they provide.
Table of Contents
ToggleUnderstanding Your Immune System: The Body’s Natural Defense Force
Before we can understand how vaccines work, we must first appreciate the incredible system they are designed to interact with: the human immune system. This complex network of cells, tissues, and organs is our personal, 24/7 security detail, constantly on patrol for foreign invaders like viruses, bacteria, fungi, and parasites. Its primary mission is to distinguish between “self” (your own healthy cells) and “non-self” (anything foreign and potentially harmful) and to neutralize any threats it identifies. This system is a marvel of biological engineering, capable of both brute-force responses and highly specific, targeted operations.
The immune system’s operations are broadly divided into two main branches. The first line of defense is the innate immune system, which you are born with. It’s a rapid, non-specific response force. Think of it as the general guards at the gate; they attack anything that looks suspicious without needing to know its specific identity. This includes physical barriers like your skin, mucus linings, and chemical barriers like stomach acid. If a pathogen breaches these barriers, innate immune cells like phagocytes rush to the site to engulf and destroy the invaders. This response is fast, but it doesn’t create lasting memory.
The real genius lies in the adaptive immune system, the second, more sophisticated branch. This is the part of the system that vaccines primarily engage. The adaptive system is slower to respond the first time it encounters a new threat, but its response is highly specific and, most importantly, it creates a long-lasting memory. This ensures that the next time the same pathogen appears, the response is incredibly swift and powerful. This “memory” is the key to long-term immunity and is the fundamental principle upon which all vaccination is built. It turns a first-time encounter into a well-rehearsed takedown.
The Key Players: B-Cells, T-Cells, and Antibodies
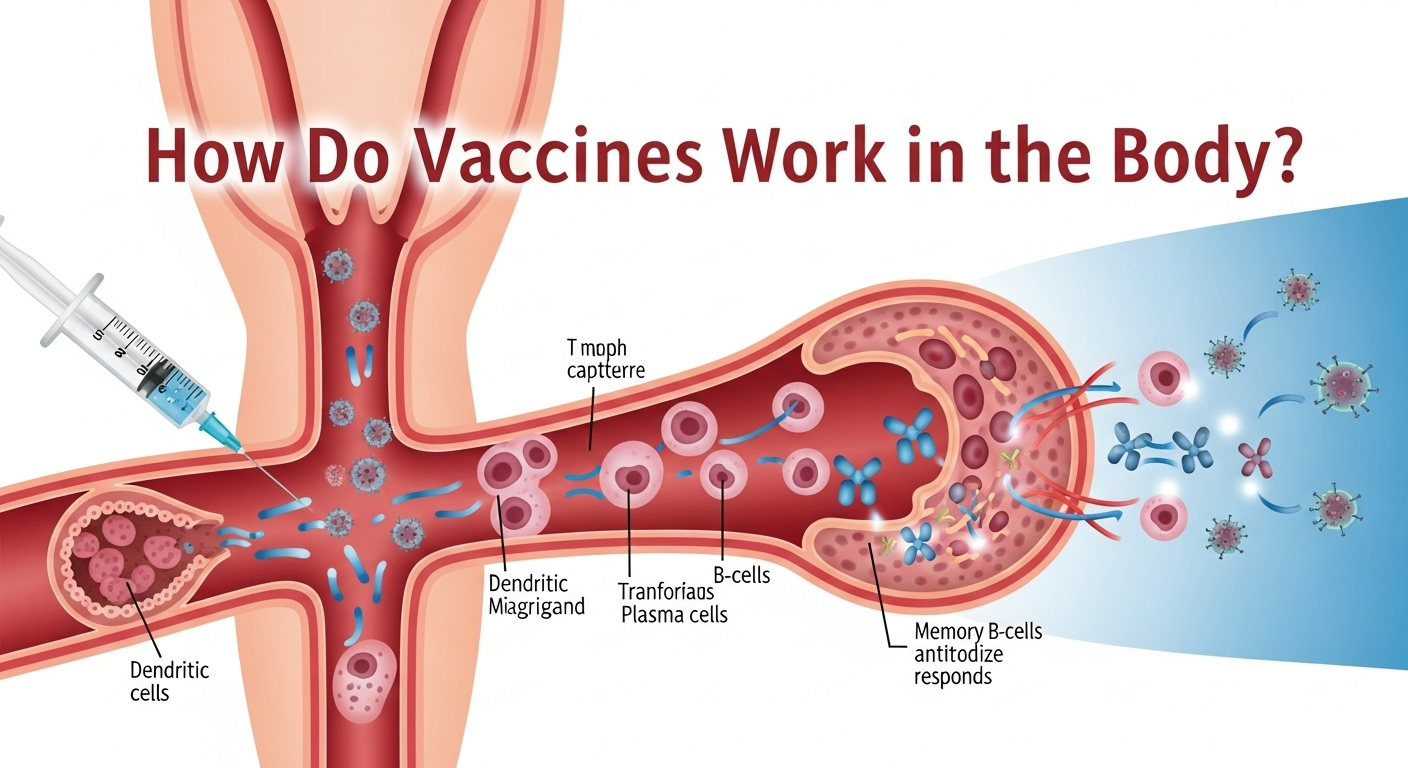
The adaptive immune system has its own set of special-forces cells, primarily lymphocytes known as T-cells and B-cells. These cells are the masterminds of the targeted response. When a vaccine introduces an antigen—a unique molecular signature from a pathogen, like a specific protein on a virus’s surface—specialized cells present this antigen to the T-cells and B-cells, effectively sounding the alarm. This kicks off a coordinated process to build a defense tailored specifically to that antigen.
B-cells are responsible for producing one of the immune system’s most famous weapons: antibodies. When a B-cell is activated by an antigen, it matures into a plasma cell and begins churning out millions of Y-shaped antibody proteins. These antibodies are like precision-guided missiles. They circulate through your blood and latch onto their specific antigen, neutralizing the pathogen in several ways. They can block the pathogen from entering your cells, mark it for destruction by other immune cells, or trigger a cascade of other defensive proteins. Some of these activated B-cells also become long-lived memory B-cells, which remain in your body for years, ready to produce a flood of antibodies instantly upon re-exposure to the pathogen.
The Role of Helper T-Cells and Killer T-Cells
While B-cells are the antibody factories, T-cells play a variety of crucial roles, acting as both commanders and front-line soldiers. There are two main types of T-cells involved in fighting infections. Helper T-cells (CD4+ cells) are the strategic coordinators. When they recognize an antigen, they become activated and release chemical signals called cytokines. These signals help mobilize and direct other immune cells, including activating B-cells to start producing antibodies and rallying Killer T-cells to join the fight. They are essential for a robust and well-organized immune response.
Killer T-cells (CD8+ cells), on the other hand, are the assassins. Their job is to find and destroy your body’s own cells that have already been infected by a virus. Viruses replicate by hijacking the machinery inside our cells. Killer T-cells are trained to recognize the tell-tale signs of an infected cell (by spotting viral antigens on the cell’s surface) and eliminate it before the virus can multiply and spread further. Just like B-cells, some T-cells also become memory T-cells, providing another layer of long-term, rapid-response surveillance against future infections.
The Core Principle of Vaccination: A “Training Session” for Your Body
Now that we understand the key players in the adaptive immune system, the logic of vaccination becomes crystal clear. A vaccine’s purpose is to trigger this entire adaptive response—the production of antibodies and the creation of memory B-cells and T-cells—without making you sick. It achieves this by introducing a safe and controlled version of a pathogen’s antigen into your body. This antigen is the “wanted poster” that teaches your immune system what the enemy looks like. It contains enough information for the immune system to learn, but it lacks the ability to cause disease.
This process is essentially a simulated battle. The vaccine introduces the antigen, and antigen-presenting cells carry it to the lymph nodes, where B-cells and T-cells are waiting. Helper T-cells are activated, which in turn signal B-cells to start producing antibodies specific to that antigen. Killer T-cells are also prepared to recognize and destroy any cells that might display this antigen. The entire cascade unfolds just as it would during a real infection, but in a completely controlled environment. The minor side effects sometimes felt after a vaccine, like a sore arm, low-grade fever, or fatigue, are actually signs that this “training session” is working and your immune system is actively building its defenses.
The most critical outcome of this training is the creation of long-lived memory cells. After the initial response to the vaccine subsides, these memory B-cells and T-cells go into a state of quiet surveillance, circulating in your body for months, years, or even a lifetime. They are the veterans of the simulated battle, holding the blueprint for defeating that specific enemy. If you are later exposed to the actual, disease-causing pathogen, these memory cells awaken immediately. They orchestrate an antibody and T-cell response that is so rapid and overwhelming that the pathogen is eliminated before it can multiply and cause illness. You gain immunity without the price of suffering from the disease itself.
A Closer Look at Different Types of Vaccines
Vaccine technology has evolved significantly over the centuries, leading to a variety of sophisticated platforms, each with a unique way of presenting antigens to the immune system. While they all share the same fundamental goal of creating immunologic memory, their methods differ. Understanding these types helps to appreciate the breadth of scientific innovation in preventive medicine.
Live-Attenuated and Inactivated Vaccines (The Classics)
These are two of the most traditional and time-tested vaccine approaches. A live-attenuated vaccine uses a version of the living virus or bacterium that has been significantly weakened (attenuated) in a laboratory so that it cannot cause disease in people with healthy immune systems. However, because it is still live and can replicate to a very small extent, it provides a very strong, comprehensive, and long-lasting immune response that is nearly identical to what a natural infection would produce. Examples include the measles, mumps, and rubella (MMR) vaccine and the chickenpox vaccine.
An inactivated vaccine, by contrast, uses a version of the virus or bacterium that has been killed, or inactivated, with heat or chemicals. Because the pathogen is dead, it cannot replicate at all, making it impossible for the vaccine to cause the disease. This also means the resulting immune response may not be as strong or long-lasting as with a live vaccine. Therefore, inactivated vaccines often require multiple doses or “booster shots” over time to maintain immunity. Well-known examples include the inactivated polio vaccine and most seasonal flu shots.
Subunit, Recombinant, Polysaccharide, and Conjugate Vaccines (The Targeted Approach)
Instead of using the entire pathogen, these more modern vaccines use only a specific piece of it—the antigen—that best stimulates the immune system. This is a highly targeted approach. Subunit vaccines contain just a specific protein or carbohydrate from the pathogen’s surface. The hepatitis B vaccine, for example, contains only a surface protein of the hepatitis B virus, which is enough to train the immune system to recognize and attack the whole virus. This design minimizes the risk of side effects.
Recombinant vaccines are a type of subunit vaccine where the antigen is produced using genetic engineering. Scientists can insert the gene that codes for the desired antigen into another harmless cell (like yeast), which then becomes a factory for producing a large supply of the antigen. Toxoid vaccines, like those for tetanus and diphtheria, are unique because they target a harmful toxin produced by the bacteria, not the bacteria itself. The toxin is inactivated to create a toxoid, which teaches the immune system to neutralize the real toxin if an infection occurs. This prevents the disease’s harmful effects without needing to fight the entire bacterium.
mRNA and Viral Vector Vaccines (The New Generation)
The most recent innovations in vaccine technology are mRNA (messenger RNA) vaccines and viral vector vaccines, which came to global prominence during the COVID-19 pandemic. These platforms represent a revolutionary approach. Instead of injecting the antigen itself, they provide your body with the genetic instructions to produce the antigen for a short period. An mRNA vaccine contains a small piece of genetic material (mRNA) encased in a protective lipid nanoparticle. Once injected, your own cells use this mRNA as a blueprint to manufacture the harmless antigen (e.g., the spike protein of the coronavirus). Your immune system then detects this foreign protein and mounts its defensive response. The mRNA itself is very fragile and is broken down by the body within a few days.
Viral vector vaccines work similarly but use a different delivery system. They use a modified, harmless virus (the “vector,” often an adenovirus) to deliver genetic instructions into your cells. This vector virus has been engineered so it cannot replicate or cause disease. It simply acts as a transport vehicle to carry the gene for the target antigen into a cell. Once inside, the cell machinery reads the gene and produces the antigen, triggering the desired immune response. The Johnson & Johnson and AstraZeneca COVID-19 vaccines are well-known examples of this technology. Both mRNA and viral vector platforms allow for rapid vaccine development and have proven to be highly effective.
From Injection to Immunity: The Timeline of a Vaccine’s Effect
After receiving a vaccine, the process of building immunity is not instantaneous; it unfolds over days and weeks as your adaptive immune system learns and prepares. Understanding this timeline can help manage expectations and clarify why you are not considered fully protected immediately after the shot. The process can be broken down into distinct phases.
The first phase is the immediate inflammatory response, which occurs in the first 24 to 48 hours. This is driven by your innate immune system. When the vaccine is injected, your body recognizes a foreign presence at the injection site. Innate immune cells are dispatched, releasing inflammatory signals that cause the common and expected side effects like redness, swelling, and soreness in the arm. Some people may also experience systemic effects like a mild fever, headache, or fatigue. These are all positive signs that your immune system has been activated and is beginning to process the vaccine’s contents.
The second, and most critical, phase is the adaptive immune response and antibody production, which typically ramps up over the following one to two weeks. During this time, the vaccine’s antigens are being presented to T-cells and B-cells in your lymph nodes. These cells begin to multiply and differentiate. Helper T-cells coordinate the response, and B-cells mature into plasma cells that start producing a large quantity of antibodies specifically designed to target the pathogen’s antigen. It is during this period that the foundation for long-term immunity is built. This is why health authorities state that it takes about two weeks after a final dose for a person to be considered fully vaccinated and protected.
| Timeframe | Primary Immune System Activity | Potential User Experience |
|---|---|---|
| 0 – 48 Hours | Innate immune system activation. Inflammation at the injection site. Antigen-presenting cells capture the vaccine’s antigens. | Soreness, redness, or swelling at the injection site. Possible mild fever, fatigue, or headache. |
| 1 – 2 Weeks | Adaptive immune system activation. B-cells and T-cells multiply. B-cells begin producing high levels of specific antibodies. | Side effects typically subside. The body is actively building its “army” of antibodies and memory cells. |
| 2+ Weeks | Peak antibody levels are reached. Memory B-cells and T-cells are fully established and enter a surveillance state. | You are now considered to have a protective level of immunity against the target disease. |
| Long-Term | Memory cells persist in the body for months, years, or a lifetime, providing long-term protection against future encounters with the pathogen. | Ongoing, durable protection. Booster shots may be needed for some vaccines to “remind” the immune system. |
The Bigger Picture: Herd Immunity and Public Health
While vaccines provide powerful protection for the individual, their true power is magnified when viewed from a public health perspective. When a large enough portion of a community is vaccinated and immune to a disease, it creates a protective shield known as herd immunity, or community immunity. This concept is crucial for protecting an entire population, especially its most vulnerable members.
Herd immunity works by breaking the chains of transmission. A contagious disease needs susceptible people to infect in order to spread. If an infected person is surrounded by immune individuals, the pathogen has nowhere to go and the outbreak fizzles out. This significantly reduces the chance that someone who is vulnerable will come into contact with the disease. The threshold of vaccination needed to achieve herd immunity varies depending on how contagious the disease is. For a highly contagious disease like measles, over 95% of the population needs to be immune to protect the community.
This community-wide protection is life-saving for people who cannot be vaccinated. This includes newborn infants who are too young for many vaccines, people with weakened immune systems (immunocompromised) due to illnesses like cancer or HIV, and individuals with severe allergies to vaccine components. These vulnerable groups rely on the immunity of those around them to keep them safe. Therefore, choosing to get vaccinated is not just a personal health decision; it is an act of social responsibility that contributes to the health and safety of your entire community, protecting friends, family, neighbors, and strangers alike.
Frequently Asked Questions (FAQ) about How Vaccines Work
Q: Can a vaccine give me the disease it’s meant to prevent?
A: No, this is one of the most common misconceptions. It is impossible for a vaccine to give you the disease it is designed to prevent. Inactivated, subunit, toxoid, and mRNA vaccines contain no live pathogen, so there is no mechanism by which they could cause an infection. Live-attenuated vaccines use a severely weakened form of the pathogen that cannot cause illness in people with a healthy immune system. The mild, flu-like symptoms some people experience after vaccination are not the disease itself, but rather the sign of a healthy immune system response being mounted.
Q: Why do I sometimes need a booster shot?
A: Booster shots serve two main purposes. First, for some vaccines (especially inactivated ones), the initial immune memory can fade over time. A booster shot acts as a “reminder” for your immune system, stimulating your memory cells to produce more antibodies and strengthening your long-term protection. Second, some pathogens, like the influenza virus, mutate and change over time. An annual flu shot is a type of booster that is updated to match the circulating strains for that year, ensuring your immune system is prepared for the most current version of the virus.
Q: Is natural immunity from getting sick better than vaccine-induced immunity?
A: While recovering from a natural infection does typically result in strong immunity, achieving it comes with the serious, unpredictable, and sometimes deadly risks of the disease itself. For example, getting “natural” immunity to measles carries a 1 in 1,000 risk of encephalitis (brain swelling) and a 1-2 in 1,000 risk of death. Vaccine-induced immunity provides a reliable and powerful immune response without you having to risk the potentially severe complications of a natural infection, including long-term health problems, hospitalization, or death. Vaccines are a much safer and more predictable path to protection.
Q: How long does vaccine immunity last?
A: The duration of immunity varies significantly depending on the vaccine and the disease. Some vaccines, like the MMR vaccine, provide lifelong or very long-lasting immunity after a full course. Others, like the tetanus vaccine, require boosters every 10 years to maintain optimal protection as antibody levels wane. For rapidly evolving viruses like influenza, annual vaccination is recommended. The longevity of immunity is a key factor that scientists study during clinical trials and post-market surveillance to establish official vaccination schedules.
Conclusion
The science behind how vaccines work is a story of preparation, memory, and empowerment. By providing our immune systems with a safe and controlled “training manual,” vaccines enable our bodies to build a robust and lasting defense against dangerous diseases without having to endure the perils of a full-blown infection. From the classic live-attenuated and inactivated platforms to the cutting-edge mRNA and viral vector technologies, the fundamental goal remains the same: to create a legion of memory B-cells and T-cells that stand ready to protect us.
This elegant biological process not only safeguards our individual health but also weaves a critical fabric of community protection known as herd immunity, shielding the most vulnerable among us. Understanding that the mild side effects of a vaccine are simply signs of a productive training session helps to demystify the experience and reinforces the trust we can place in this life-saving medical intervention. Ultimately, vaccination stands as one of humanity’s most effective strategies for preventing suffering and promoting a healthier future for everyone.
***
Article Summary
This article, “How Do Vaccines Work in the Body? A Simple Explainer,” provides a comprehensive overview of the science behind vaccination. It begins by explaining that vaccines act as a “training session” for the body’s adaptive immune system, allowing it to build memory and defenses against a pathogen without causing illness. The article first details the key components of the immune system, including the innate and adaptive branches, and the crucial roles of B-cells (which produce antibodies) and T-cells (which coordinate the response and kill infected cells).
The core of the article breaks down the different types of vaccines, from traditional live-attenuated and inactivated vaccines to more targeted subunit and toxoid vaccines, and finally to modern mRNA and viral vector platforms. It explains the unique mechanism of each type, highlighting their shared goal of safely introducing an antigen to create memory B-cells and T-cells. The article includes a table illustrating the timeline of the immune response post-vaccination, from immediate inflammation to the two-week period required to build full immunity. It also addresses the critical public health concept of herd immunity, emphasizing how widespread vaccination protects the most vulnerable members of a community. Finally, a detailed FAQ section answers common questions regarding vaccine safety, booster shots, and natural vs. vaccine-induced immunity, culminating in a conclusion that reinforces vaccines as a safe, effective, and essential tool for preventive public health.